
Identifying areas with limited spatial accessibility of health care services allows planners to understand the effects of opening, closing, or relocating health care facilities or modifying the services offered by existing facilities. Accessibility (or geographic accessibility) is a measure of the “friction of distance” or “burden of travel” between locations, whereas availability generally measures the number of services in comparison to the number of potential users of the service. Referred to as spatial accessibility, the spatial dimensions of access include accessibility and availability of services. The spatial or geographic dimensions of access have received considerable attention from planners and researchers for many years. These populations experience greater difficulty in gaining access due to increased travel times, often coupled with poor transportation infrastructure and a lack of public transportation options. Of particular concern are scenarios that result in large distances between people and health care facilities. Although inequalities in accessibility are inevitable due to this configuration, the extent to which they manifest is a product of the unique spatial arrangement of the health care delivery system, the location and distribution of the population within a region, and the characteristics of the transportation infrastructure.

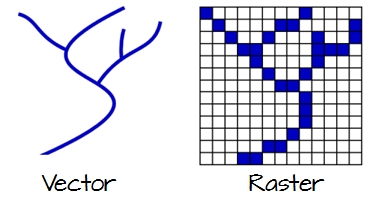
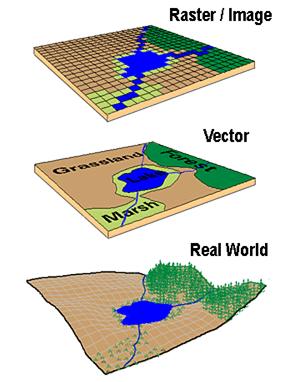
Specifically, health care services are provided at a finite number of fixed locations, yet they serve populations that are continuously and unevenly distributed throughout a region. Additionally, we recommend that the state revisit the population assignment method.ĭisparities in the geographic accessibility of health care services arise due to the manner in which people and facilities are arranged spatially. For policy, we recommend that Michigan adopt the network-based method or reevaluate the travel speed assignment rule in the raster-based method. Considering that the choice of data model/method may substantially alter the outcomes of a geographic accessibility analysis, we advise researchers to use caution in model selection. Conclusionsĭifferences between the underlying data models help to explain the variation in results between raster and network-based methods. The raster-based method was more sensitive to travel speed settings, while the network-based method was more sensitive to the specific population assignment method employed in Michigan. Over all permutations, the raster-based method identified more area and people with limited accessibility. However, the number of people identified as having limited accessibility varied substantially between methods. In both methods, the areas identified as having limited accessibility were similar in their location, configuration, and shape. We also examine sensitivity to changes in travel speed settings and population assignment. Both network and raster-based methods are implemented and their results are compared. Geographic accessibility is calculated by identifying the number of people residing more than 30 minutes from an acute care hospital. Our case study investigates Limited Access Areas defined by Michigan’s Certificate of Need (CON) Program. Conceptual and practical differences between raster and network data models are reviewed, along with methodological implications for service area estimates. We examine the assumptions present in population-based travel time models. Therefore, exploring the differences in the underlying data models and associated methods and their impact on geographic accessibility estimates is warranted. Both network and raster-based methods are often utilized for estimating travel time in a Geographic Information System. In recent accessibility studies, the traditional distance measure (Euclidean) has been replaced with more plausible measures such as travel distance or time.
Inequalities in geographic access to health care result from the configuration of facilities, population distribution, and the transportation infrastructure.


 0 kommentar(er)
0 kommentar(er)
